Plastic & Reconstructive Surgery
- Breast
- Facial Paralysis
- Diabetic foot
- Hand
- Facial fracture
- Microtia
- Congenital giant nevus
- Skin cancer
- Lymphedema
Why Plastic & Reconstructive Surgery in Korea
-
Plastic Surgery is often referred to as Plastic & Reconstructive Surgery, and sometimes ‘aesthetic’ is preferred to ‘plastic’.
While Reconstructive Surgery is restoring damage or defects to a normal state, aesthetic surgery is improving the normal state.
Recently Reconstructive Surgery has developed to be widely applied across all areas of medicine, including treatment of tissue defects caused by trauma and congenital deformities, as well as reconstruction after cancer surgery and treatment of incurable diseases.
-
- Unlike other surgeries, breast cancer surgery should consider aesthetic aspects to preserve a natural-looking breast on top of removing cancer cells. Broadly speaking, breast reconstruction has two different approaches: autologous tissue transplantation and prosthetic implants. Recently, advanced devices such as endoscopes and robots have been gradually used.
Autologous Tissue Transplantation
- Deep inferior epigastric perforator (DIEP) Blood vessels, skin and fat are taken from the lower abdomen and used to reconstruct a breast
- Latissimus dorsi flap (LD flap) Blood vessels, skin and fat are taken from the back and used to reconstruct a breast
- Profunda Femoris Artery Perforator Flap breast reconstruction (PAP) Tissues are used from the inner thigh and inner and lower buttock to reconstruct a breast : For patients who find it difficult to use abdominal tissue, breast reconstruction is available using autologous tissue from other areas (thighs, buttocks, flanks, etc.). Recently, PAP flap using thigh tissues has been popular as the latest approach.
Prosthetic Implants
- Prosthetic implants are a method of replacing the breast tissue removed from total mastectomy with an implant to restore it to the original breast shape or make it look symmetrical with the other side.
- It is a simple surgery compared to the one using autologous tissue, considering that it takes only one to two hours.
The patient can expect a quick recovery and the hospital stay is relatively short.
Breast Reconstruction using Robots
- For robot-assisted breast cancer surgery, a surgeon creates a minimal incision near the patient’s armpit and then inserts a robot arm into the incision to remove cancer cells. It is advantageous for preserving the natural breast shape as it minimizes scarring. Patients express high satisfaction as it helps preserve their natural breasts as much as possible.
- The Da Vinci surgical system is an advanced medical device for robot-assisted minimally invasive surgery.
A surgeon operates surgical instruments through a console using the robot. While each Da Vinci surgical system has its unique patient cart depending on the model, all systems assist surgeons in performing minimally invasive surgeries.

<Da Vinci robotic system. SI, X, XI, SP model>
-
-
Facial paralysis happens when the facial nerve that moves facial muscles does not function as expected.
By losing essential muscles that control nasal and oral functions, it can cause a complex clinical problem that affects many aspects; loss of speaking ability, self-image, and social interaction. Considering this complexity of facial paralysis, researchers strive to find and develop new and effective treatment methods.
Congenital facial paralysis
- It occurs from birth and is the most common type in pediatric patients. Usually it is not related to specific diseases but it can be accompanied by a syndrome. Sometimes it occurs separately. Approximately 2.0% of newborns experience congenital facial paralysis.
Acquired facial paralysis
- It can occur on one side or both sides. Its impact can vary depending on the affected nerve. The most common causes of acquired facial paralysis are intracranial and extracranial neoplasms, Bell's palsy, and trauma.
- Idiopathic facial paralysis (Bell’s palsy)
For the patients who suddenly develop facial paralysis, it is difficult to find a specific cause even after exams and tests.
These cases are called idiopathic facial paralysis or Bell's palsy. It is named after the British physician, Charles Bell.
Since then, it has become a widely used medical term, and it is the most common cause of facial paralysis. - Facial paralysis with an identified cause
When a specific reason for facial paralysis is found, treatment can vary depending on each cause.- Ramsay Hunt syndrome: Facial paralysis is accompanied by the Herpes Zoster virus
- Trauma: Shock, such as a car accident or fall, leads to a fracture of the skull and paralysis.
- Cranial nerve diseases: Paralysis occurs due to nerve diseases including a stroke or brain tumor.
- Complications: Facial paralysis is the result from acute or chronic otitis media.
Treatment
- Non-surgical treatment
- Bell’s palsy
A specialist monitors for several months its progress while they administer medication along with physical therapy including electrical stimulation. In more than 8 out of 10 patients with Bell's palsy, facial movements completely return to normal with just medication and monitoring. Usually it takes several months to notice its gradual recovery and some degree of paralysis remains. During follow-ups, patients may have a prescription for eye drops in order to prevent complications from dry eyes. - Ramsay Hunt syndrome
Antiviral drugs and painkillers are prescribed. In general, patients wear an eye patch to protect their eyes and do physical therapy to the paralyzed area. Treatment should begin immediately after onset and proceed with conservative therapy that facilitates blood circulation to the facial nerve. - Surgical treatment
Surgical approaches cover eyebrow correction, upper eyelid correction, lower eyelid correction, lip and isthmus correction, nerve transmission, micro-neurovascular muscle transplantation, local muscle transfer, and others. These surgeries can help repair damaged nerves or connect other nerves. In case of chronic paralysis, a surgeon can reroute healthy muscles to the affected side to restore facial movement. -
Inability to close eyes
When facial nerves are paralyzed, a patient is unable to blink eyes and the eyelids can no longer protect them.
If the eye dries and the cornea is damaged, blindness may occur. To prevent this, weights made of gold or platinum are inserted into the eyelids to ensure that a patient can control the eyelids well. -
Facial expressions
It is very challenging to restore facial expressions. Even after surgery, delicate facial expressions cannot be fully recovered. When a sagged mouth or an asymmetrical eye is noticed, a lifting procedure can help correct them. For normal facial expressions, it is necessary to repair nerves or muscles through surgery. If it has not been long since the facial nerve was damaged and the facial muscles are not contracted, the nerve can be restored through nerve transplantation.
-
Facial paralysis happens when the facial nerve that moves facial muscles does not function as expected.
-
- Recently, the number of diabetic patients has been gradually increasing. According to the World Health Organization (WHO), 5-10% of adults have diabetes and 15-25% of diabetic patients are reported to suffer from diabetic foot disease. Diabetic foot disease is a general term that handles nerve disease, structural deformation, skin changes, foot ulcers, infection, and vascular disease, all of which can occur to diabetic patients’ feet. It is a serious diabetic complication that may eventually require foot amputation.
Assessment
- Through transcutaneous oxygen monitoring (TcOM) or transcutaneous oxygen pressure (TcpO2), Peripheral Vascular Disease (PVD) severity can be assessed.
To help treat the patients with diabetic foot or severe lower extremity ischemia, enough blood must be provided to the injured area, in which oxygen can reach the wound and the cells can be restored. To ensure oxygen supply to cells, a surgeon makes a hole into arteries in the leg by applying a balloon expansion procedure or connects blood vessels by operating vascular bypass surgery.
One way to check the result is to measure oxygen partial pressure from foot tissue, as displayed in the photo below. It is reported that the wound has a better chance of healing when the oxygen partial pressure exceeds 40mmHg.

<Transcutaneous Oxygen Monitoring>
Treatment
- Negative-Pressure Wound Therapy [NPWT]
It aids cell regeneration by sealing the wound and removing necrotic tissue and exudate from the affected area while a surgeon consistently applies negative pressure. - Growth Factor Therapy
It is effective for diabetic patients who have difficulty healing wounds due to decreased growth factors. A physician directly applies growth factors for wound healing, including platelet-derived growth factor [PDGF], basic fibroblast growth factor [bFgF], and epithelial cell growth factor and Epidermal growth factor [EGF] - Cell Therapy
The goal of cell therapy is to provide a healing environment to wounds to ensure healing optimization by transplanting cells with excellent healing ability into the wound. Currently, fibroblasts, keratinocytes, adipose-derived stromal vascular fraction cells, platelet concentrates, and mesenchymal stem cells are actively used in clinical practice. - Ultrasound Therapy
Ultrasound improves wound healing by generating a thermal effect locally.
It aids in wound contraction, collagen deposition, granulation tissue formation, angiogenesis and scar flexibility. - Hyperbaric Oxygen [HBO] Therapy
Its goal is to provide 100% oxygen at a pressure more than twice the normal atmospheric pressure.
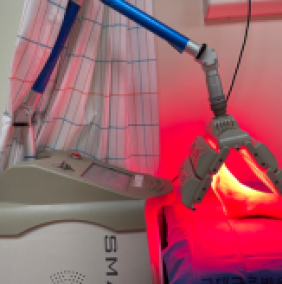
It directs more oxygen to tissues by increasing the partial pressure of oxygen dissolved in plasma. - Monochromatic Infrared Energy [MIRE] Therapy
It aids increasing nitric oxide (NO) levels in blood and plasma by delivering near-infrared energy with a wavelength of 890 nm to the skin. MIRE therapy improves cell proliferation and blood flow in the treatment area by up to 400%. - Non-invasive pain-free signal therapy, Pain Scrambler Therapy
This therapy is approved by US FDA (Food and Drug Administration) and certified by European CE marking.
It is a unique, technologically advanced treatment for chronic pain management. Pain Scrambler Therapy helps patients avoid harmful and fatal side effects associated with narcotic painkillers. - Extracorporeal shockwave therapy [ESWT]
A specialist applies shock wave energy to the painful area to restore damaged cells and increase blood flow to help the process of tissue regeneration. It is effective in inflammation treatment and reducing pain so it aids improving strengths of tendons, ligaments, and muscles.
Treatment : Hyperbaric Oxygen [HBO] Therapy, Monochromatic Infrared Energy[MIRE] Therapy, Pain Scrambler Therapy, Extracorporeal shockwave therapy Hyperbaric Oxygen [HBO] Therapy Monochromatic Infrared Energy[MIRE] Therapy Pain Scrambler Therapy Extracorporeal shockwave therapy 


-
- Considering that the hand is always exposed to the outside and handles various tools, it seems to experience more damage than other body parts. Since the operation microscope was introduced in the 1950s, the hand reconstruction has been rapidly developed and now Free Flap and Replantation procedure is more available.
As known for their delicate manual skills, Korean surgeons have performed highly challenging procedures and reconstruction surgery of multiple injuries, which were not achieved in other countries. Even in cases of amputated fingers, the surgeon finds and reconnects blood vessels of 0.2 to 0.3 mm. It requires extreme concentration with rich experience, but this happens more commonly in Korea.
Procedures
- Thumb reconstruction
Given that the thumb is responsible for 50% of all hand functions, its damages can lead to losing many functions of hands. Therefore, thumb reconstruction is critical for maintaining quality of life. There are various reconstruction methods.
The best option can be selected depending on the amputated part, the surgeon's skill, and the preferred method.- Index finger pollicization: When the thumb is amputated near the middle finger joint, the index finger pollicization is most appropriate. The index digit has a good length and the reconfigurable intrinsic muscle function with nerves remaining intact, so the pollicization surgery provides advantages that a patient does not have to go through another microsurgery and can have normal sensation back immediately. Many patients do not prefer this method due to an aesthetic reason, but its advantages outdo disadvantages. This method is also recommended for patients who were born without a thumb.
- Toe to Hand Transfer: It is used to replace part or all of the missing digit. It is a complex surgery because it needs suturing the toenail, skin, bones, nerves, and blood vessels of the toe. Depending on the severity of loss, part or all of the big toe is transferred. The big toe can be used, but mostly the second toe is preferred.
If two or more fingers are lost, the second toes on both sides may be transferred or the second and third toe are used at the same time. Recently, due to the difference in the shape of the fingernails and toenails, combining the nail of the big toe and the joint & bone of the second toe has been applied. - Free flap reconstruction: This is a method of creating a structure similar to the thumb, in which a surgeon raises the flap with bone, wraps it into a cylindrical shape, fixes it to the remaining bone of the thumb, and then connects the arterial and venous nerves. It can be less aesthetically pleasing than finger or toe transfer procedures since nails, an important part of the finger shape, cannot be made. However, it has the advantage of avoiding damage to fingers or toes.
- Extension of digits: In this procedure, a surgeon extends the first metacarpal bone using an expander. Considering a patient should wear an expander for a long time, it has the disadvantage of being vulnerable to infection, but it has the advantage of providing normal sensation and does not leave scars on other areas.
- Replantation of digits
- Finger reattachment: It has become a common procedure to replant an amputated finger. The success rate reaches over 90% if the damage to the amputation site is not severe.
- Fingertip replantation: It used to be avoided due to the technical difficulty of suturing very tiny blood vessels but recently it has become a common procedure. To ensure the recovered hand works properly, restoring the function of joints, tendons, and nerves is essential.
- Defect reconstruction
- If the amputated part of the hand is available, it can be replanted. However, if there is a defect, a surgeon uses a similar tissue to reconstruct the lost part. As the hand is composed of various tissues including bones, nerves, blood vessels, and tendons, each part can be reconstructed separately based on its importance.
- Hand deformity reconstruction
- Reconstruction surgery handles various deformities; nonunion due to improper healing of the fracture, nonunion due to improperly shaped union, deformity due to joint damage or loss, post-traumatic skin contraction, and hypertrophic scarring.
- Burn damage reconstruction
- Hands are at high risk of burns. Damage from burns can lead to serious contraction, causing bad disability. In the case of post-burn contracture, a surgeon performs reconstruction procedure, using a full-thickness graft from the groin. If symptoms are severe, a surgeon may operate free flap surgery.
- Nail reconstruction
- At the tip of each finger, nails assist the work of the hand and also provide an aesthetic aspect. When nails are damaged, depending on its severity, a surgeon applies toenail transplantation or performs microsurgery that utilizes the part around the toenail. It must be carefully opted in with sufficient understanding of the variability of outcomes; transplanted nails may not grow properly or may grow at different rates.
- Considering that the hand is always exposed to the outside and handles various tools, it seems to experience more damage than other body parts. Since the operation microscope was introduced in the 1950s, the hand reconstruction has been rapidly developed and now Free Flap and Replantation procedure is more available.
-
A. Orbital Fracture
- It is one of the most challenging procedures in facial trauma surgery as it is not easy to access, located deep in the orbital bone. A surgeon should be careful not to damage any part of various important structures, including the optic nerve.
- The repair procedure of orbital fracture mainly aims to reposition the herniated contents in the eye and prevent further fractures.
How to reconstruct
- Orbital wall restoration using primary bone fragments
A surgeon repositions the fractured orbital bone fragment transnasally in addition to the transorbital approach. Then, the surgeon places a temporary support on the maxilla and ethmoid sinus until the orbital wall bones are properly fused. - Medial orbital wall fracture restoration
To reconstruct a large bone defect from a medial lower orbital wall fracture, a surgeon should use a large prosthesis that can connect both ends of the bone in the defect. For orbital fracture repair, it is necessary to take an open approach and utilize orbital wall support.
How to reconstruct : Medial orbital wall fracture, Inferomedial strut destroyed by inferomedial wall fracture cannot be reconstructed by an intraocular approach, An extraorbital support is essential for reconstruction of inferomedial wall fracture. Medial orbital wall fracture Inferomedial strut destroyed by inferomedial wall fracture cannot be reconstructed by an intraocular approach An extraorbital support is essential for reconstruction of inferomedial wall fracture. 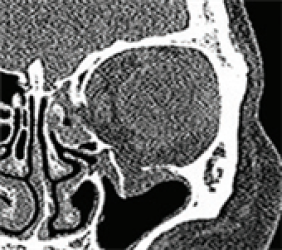
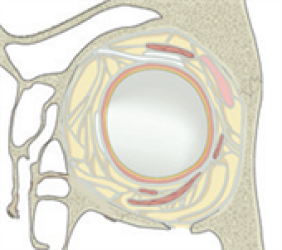

- * Broadly, there are 3 different open approaches for surgical fracture treatment; conjunctival incisions, lower eyelid incisions, and transmaxillary sinus approaches through intraoral incisions. In addition, a coronal incision enables a surgeon to access the inner, superior, and outer walls of the orbit. A surgical procedure using endoscopic orbital approaches can also be an option.
B. Facial fracture
- Facial fractures are mainly caused by traffic accidents, industrial disasters, various accidental happenings, and violence. It occurs overwhelmingly in young and middle-aged men, and also frequently occurs in growing children. Recently, fracture accidents have been on the rise due to the increasing popularity of outdoor activities and sports.
Treatment
- Endoscopic treatment for lower jaw fractures
For lower jaw fractures, they account for 25% to 45% of all fractures. They can be treated by using various methods, including retromaxillary, premaxillary, and mandibular approaches. However, there are potential possibilities of complications including facial scarring, facial nerve trauma, bleeding due to artery rupture, and avascular necrosis of the proximal segment.
To treat cartilage fractures of the lower jaw, the endoscopic-assisted transoral approach is a minimally invasive surgical procedure. This technique leaves little facial scarring and the risk of damage to the facial nerve is very low.- Carotid endoscopic approach
- Submandibular endoscopic intraoral approach
- Orbital fracture surgery with a navigation system
The surgical navigation system provides detailed preoperational analysis, virtual planning of procedures, guidance & control during operation, and post operational validation. The intraoperative navigation system assists with real-time confirmation of implant placement through CT scans and 3D screens.- Benefits of the intraoperative navigation system
- - Minimally invasive approach
- - Minimal regional craniotomy through comminuted fracture site
- - Avoidance of bi-ductal incision
- - Safe dissection
- - Short surgery time
- - Robust implant placement
- - Maintaining facial symmetry
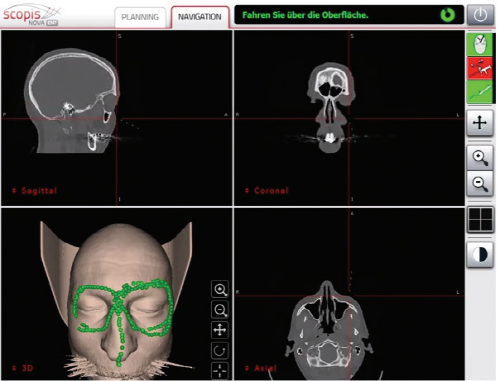
<The navigation system interface screen is divided into four views: coronal, sagittal, axial and three-dimensional>
-
- Congenital microtia (anotia) is a deformity that occurs when the ear tissue is not sufficiently developed in the early fetal period. When any trace of the outer ear remains, it is called microtia. With no trace, it is anotia.
Surgery
- Until the early 1990s, a surgeon used breast cartilage based on the size of the ear in 8-year-olds. Recently, procedures have been developed to create ears that are almost similar to normal ears by reconstructing the ears in the form of ear holes, ear lobes, and protruding ear structures. To perform these procedures, a greater amount of chest cartilage is required than before.
Now the surgery timing is determined based on the growth of breast cartilage, and the procedure is recommended for those who are over 12 years old with the chest circumference 75cm and the height 155 cm or more.
Surgery : Category, Details, Hours for Surgery, Postoperative care Category Details Hours for Surgery Postoperative care 1st operation As a procedure to create the overall frame of the ear, a surgeon removes chest cartilage in order to create an ear cartilage frame and then plants it in the area to be reconstructed for microtia. Around 5 hours (General Anesthesia) Hospital stay: 10 days Outpatient treatment: 30 days (2 times a week) 2nd operation The surgeon creates an ear that protrudes to the same height as the other ear so that both ears are visible from the front. It can be performed approximately 6 months after the first operation. Around 3.5 hours (General Anesthesia) Hospital stay: 7 days Outpatient treatment: 20 days (2 times a week) 3rd operation The surgeon refines the shape of the ear to look as similar as possible to the other ear. It can be performed approximately 4 to 6 months after the second operation. Around 3.5 hours (Local Anesthesia) Hospital stay: Not applicable (Discharge on the same day) Outpatient treatment: 30 days Surgery : Before, After, The other normal ear Before After The other normal ear 








-
- Congenital giant nevus refers to a congenital melanocytic nevus whose long axis is more than 50 cm in size. Congenital nevus is a birthmark that a baby is born with, and its prevalence is about 1% of all newborns. Although rare, it can cause ‘malignant melanoma’, a skin cancer, so early diagnosis and treatment are important.
Treatment
- Serial resection
It is applied when the size of the nevus is relatively large and requires 2-3 excisions. The procedure is usually performed at intervals of 3 to 6 months. - Skin grafting
This is a method to reconstruct the resected defect with skin grafting after surgery. While a single procedure is usually sufficient, new scars may develop at the skin graft donor site or contracture scars may form at the transplant site over time. - Tissue expansion surgery
This is the most commonly used method for giant nevus. The procedure involves inserting an expander into the surrounding skin without a nevus and expanding it as much as possible. Following this expansion, the nevus is removed and the expanded normal skin is transferred to be reconstructed.- First operation: A surgeon inserts a tissue expander under the normal skin tissue around the nevus. Afterwards, using saline solution or air injection, the surgeon expands the tissue expander for at least 3 to 6 months. The nevus is removed by expanding the area of the outer skin.
- Second operation: Once the skin expansion is complete, the birthmark is removed and the excised area is covered with expanded skin tissue.
- Non-surgical treatment
Depending on the depth and size of the nevus, a surgeon may treat it with laser therapy (CO2 laser, Nd-YAG laser), cryotherapy, and electrodrying. In laser treatment, the nevus may not be removed all at once, and the effect may be observed in stages. If the result is not successful after initial laser treatment, surgical treatment may be required.
-
- The skin is made up of three layers, in order from the surface; the epidermis, the dermis, and the hypodermis, as known as the fat layer. Skin cancer can occur in all tissues and cells that make up the skin. Common cases of skin cancer include basal cell carcinoma, squamous cell carcinoma, and melanoma. In addition, there are rare skin cancers such as angiosarcoma, dermatofibrosarcoma protuberans, Paget's disease of the papilla, and skin adnexal cancer.
- Basal cell carcinoma (BCC)
As the most common type of skin cancer, it often occurs on the face, especially around the nose, eyelids, and cheeks. They grow slowly and rarely spread to other parts of the body. However, there is a possibility of local invasion into the surrounding skin, subcutaneous tissue, muscles, and even bones.
* Surgical method Surgical resection, Mohs microscopic surgery, curettage and electrocautery, cryosurgery - Squamous cell carcinoma (SCC)
Squamous cell cancer occurs most commonly in the face, lower lip, and ears. It usually occurs in areas where there were actinic keratosis, burn scars, or chronic ulcers. Compared to basal cell carcinoma, it is more likely to metastasize to other areas. - Malignant melanoma
It mainly occurs in melanocytes in the basal layer of the epidermis, and there are notable variations in its primary site and prevalence based on race. Given its high malignancy and potential for early-stage metastasis to other organs, prompt diagnosis and complete surgical resection are imperative. - Other cancers
- Angiosarcoma (AS) is a malignant tumor from the endothelial cells of blood vessels or lymphatic vessels. Its treatment involves surgical resection or radiation therapy.
- Dermatofibrosarcoma protuberans (DFSP) is a rare form of skin cancer that begins in connective tissue cells in the middle layer of the skin. It resembles a pimple and appears on the arms, legs, and torso, growing slowly.
- Extramammary Paget’s disease (EMPD): It primarily occurs in the nipples. EMDP results from the spread of mammary duct cancer to the skin of the nipples.
- Sebaceous carcinoma: It arises in sebaceous cells in the dermis and subcutaneous tissue of the skin, mainly manifesting around the eyes, face, scalp, and neck.
- Liposarcoma: It is a malignant tumor composed of fat cells that develops in the body's fat tissue. It frequently occurs in tissues under the skin with normal fatty tissue, such as the torso, lower limbs, and arms.
- Subungual melanoma (SUM): This type of melanoma is characterized by black lesions found on the nails. Although rare, the prognosis is generally poor, necessitating a biopsy for accurate diagnosis.
Diagnosis
- To accurately diagnose skin cancer, a skin biopsy is performed under local anesthesia, removing and examining a part of the skin lesion. Detailed examinations, including chest X-ray, abdominal ultrasound, CT, and MRI, are recommended to assess the level of spread including the depth of tumor invasion and the extent of metastasis. n particular, for melanoma, which is the most malignant form, a specialist may select the ABCD observation method.
- ABCD Observation Method
- - Asymmetry: Examining whether one half of the lesion differs from the other half.
- - Border Irregularity: Assessing the edges for irregularities.
- - Color Variegation : Observing for variations in color within the lesion.
- - Diameter: Checking if the diameter exceeds 0.6 cm.
Treatment
- Surgical resection, Mohs microscopic surgery (a special surgical method designed to effectively and completely remove skin cancer)
- Cryotherapy, Photodynamic therapy: Applicable for early stage skin cancer
- Radiation therapy: Suitable for elderly patients for whom surgical operation is difficult
- Anticancer treatment, Targeted anticancer drugs, Immune anticancer drugs: Applicable for patients with metastasis
-
- Lymphedema occurs when lymphatic vessels are damaged and fluid containing protein builds up in soft body tissues. It causes swelling and chronic inflammation in the arms or legs. There are two main types of lymphedema. The primary type occurs shortly after birth with unknown cause. The secondary occurs after surgery, radiation therapy, or trauma. Both symptoms get worse over time, so early diagnosis and treatment are necessary.
Diagnosis
- Limb circumference/volume measurement: After the volume of the limb is examined, the normal side can be compared with the other side.
- Lymphoscintigraphy: As a nuclear medicine test, a specialist injects a radioisotope between the toes or fingers and takes an imaging of lymph fluid flow.
- Ultrasound exam: A specialist checks the thickness and hardness of the skin and subcutaneous tissue.
Treatment
- Conservative treatment
- Physical therapy: It aims to remove edema and involves skin care, lymph absorption massage, compression therapy, and exercise therapy.
- Local hyperthermia: A doctor applies heat to the target area.
- Medication
- Surgical treatment
- Lympovenous bypass: A surgeon creates a path to aid lymphatic circulation by connecting lymphatic vessels less than 0.7mm under the skin to the veins using a microsurgical method.
- Lymph node transplant: A surgeon transplants healthy lymph nodes to the edematous site.
- Liposuction: This surgical approach aims to reduce the edema itself to address chronic lymphedema and severe fibrosis, given that the lymphatic function is significantly compromised, and conservative therapies are less effective. It entails removing the excessively accumulated subcutaneous tissue along with the skin in the affected area. The goal is to achieve reduction in circumference and volume, thereby alleviating the symptoms of lymphedema.
- * Considering the unique characteristics of the disease, lymphedema requires a systematic approach from diagnosis to surgery and rehabilitation. The medical system in South Korea has a well-established interdisciplinary system, providing excellent medical care service in treating lymphedema. The specialists with extensive experience in microsurgery successfully deliver satisfying results.